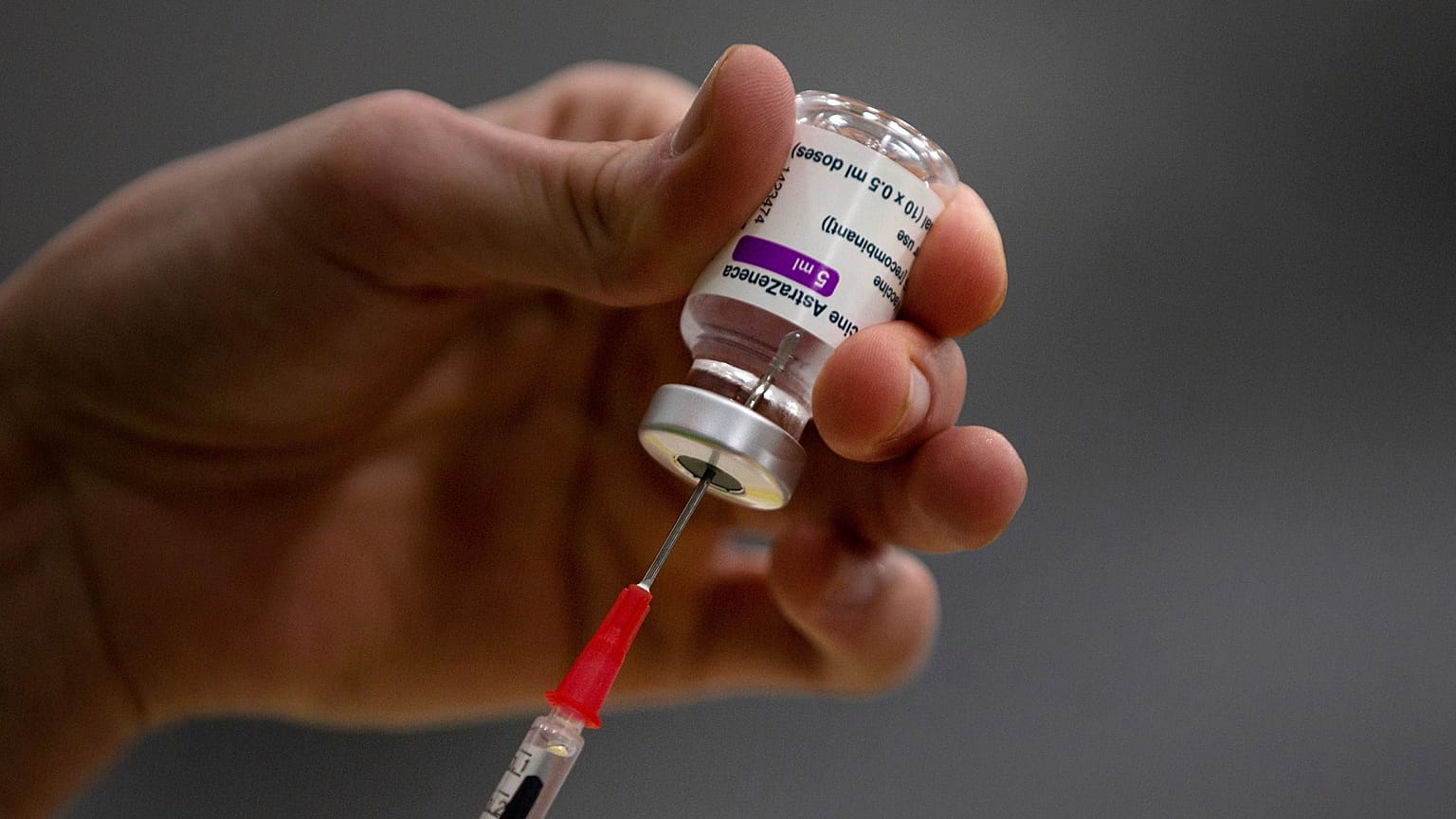
The AstraZeneca and Johnson & Johnson coronavirus vaccines are associated with extremely rare cases of blood clots - and now scientists think they may know what’s behind this.
Scientists believe they may have the answer as to why some coronavirus vaccines are associated with extremely rare cases of blood clots.
 ADVERTISEMENT
ADVERTISEMENT
 ADVERTISEMENT
ADVERTISEMENT
In a peer-reviewed paper published in the international journal Science Advances on Wednesday, the team behind the research say they think they have pinpointed a "molecular mechanism" behind the clots linked to adenovirus vaccines, such as AstraZeneca and Johnson & Johnson.
A number of European countries halted the use of AstraZeneca’s vaccine earlier this year due to reports of rare blood clotting events, while earlier this week Slovenia stopped the use of Johnson & Johnson for good following the death of a 20-year-old woman in September.
A team of researchers from Arizona State University and Cardiff University says the rare blood clot condition, termed vaccine-induced immune thrombotic thrombocytopenia (VITT), "only happens in extremely rare cases because a chain of complex events needs to take place to trigger this ultra-rare side effect".
The paper explains that the cause of VITT in extremely rare cases could be down to the adenovirus used in the vaccines - which carries genetic information into cells - and the immune response to this.
"We hope our findings can be used to better understand the rare side effects of these new vaccines – and potentially to design new and improved vaccines to turn the tide on this global pandemic," Professor Alan Parker, an expert in the use of adenoviruses for medical applications from Cardiff University’s School of Medicine, said.
How do the vaccines potentially cause VITT in rare cases?
They believe the use of the ChAdOx1 adenovirus - used in the AstraZeneca vaccine to deliver genetic information into cells - could hold the key.
The team hypothesised that in rare cases the adenovirus may then bind to a certain protein called platelet factor 4 (PF4), which triggers an immune reaction. That reaction leads to antibodies binding to the protein, causing them to cluster, and in extremely rare cases, cause VITT.
"It’s really critical to fully investigate the vector-host interactions of the vaccine at a mechanistic level," said Abhishek Singharoy, an Arizona State University scientist and corresponding author of the study.
"This will assist in understanding both how the vaccine generates immunity, and how it may lead to any rare adverse events, such as VITT".
"VITT only happens in extremely rare cases because a chain of complex events needs to take place to trigger this ultra-rare side effect," Parker added.
"Our data confirms PF4 can bind to adenoviruses, an important step in unravelling the mechanism underlying VITT. Establishing a mechanism could help to prevent and treat this disorder".