Studies show girls vaccinated by age 16 face dramatically lower cervical cancer risk with no major side effects.
The HPV vaccine is highly effective at preventing cervical cancer and does not come with serious side effects, according to two sweeping new reviews that offer some of the most comprehensive data yet on the jab.
 ADVERTISEMENT
ADVERTISEMENT
 ADVERTISEMENT
ADVERTISEMENT
Girls aged 16 or younger who received the human papillomavirus (HPV) vaccine were 80 per cent less likely to develop cervical cancer than unvaccinated girls, the analyses found.
The jab also prevented precancerous changes in the cervix and other tissue, especially when young people received it before they were exposed to the virus.
The reviews were carried outby Cochrane, an influential nonprofit research group. They included both clinical trials and real-world studies involving more than 132 million people.
“We now have clear and consistent evidence from around the world that HPV vaccination prevents cervical cancer,” Nicholas Henschke, one of the study’s authors and head of Cochrane Response, said in a statement.
HPV is a family of common viruses – many of which are harmless, including those causing skin warts. But certain forms of the virus can cause cancers of the cervix, anus, penis, vulva, vagina, mouth and throat, as well as genital warts.
Cervical cancer is among the most common cancers in women, with about 660,000 new cases and around 350,000 deaths worldwide in 2022, according to the World Health Organization (WHO). It disproportionately affects younger women.
Interrogating fears over side effects
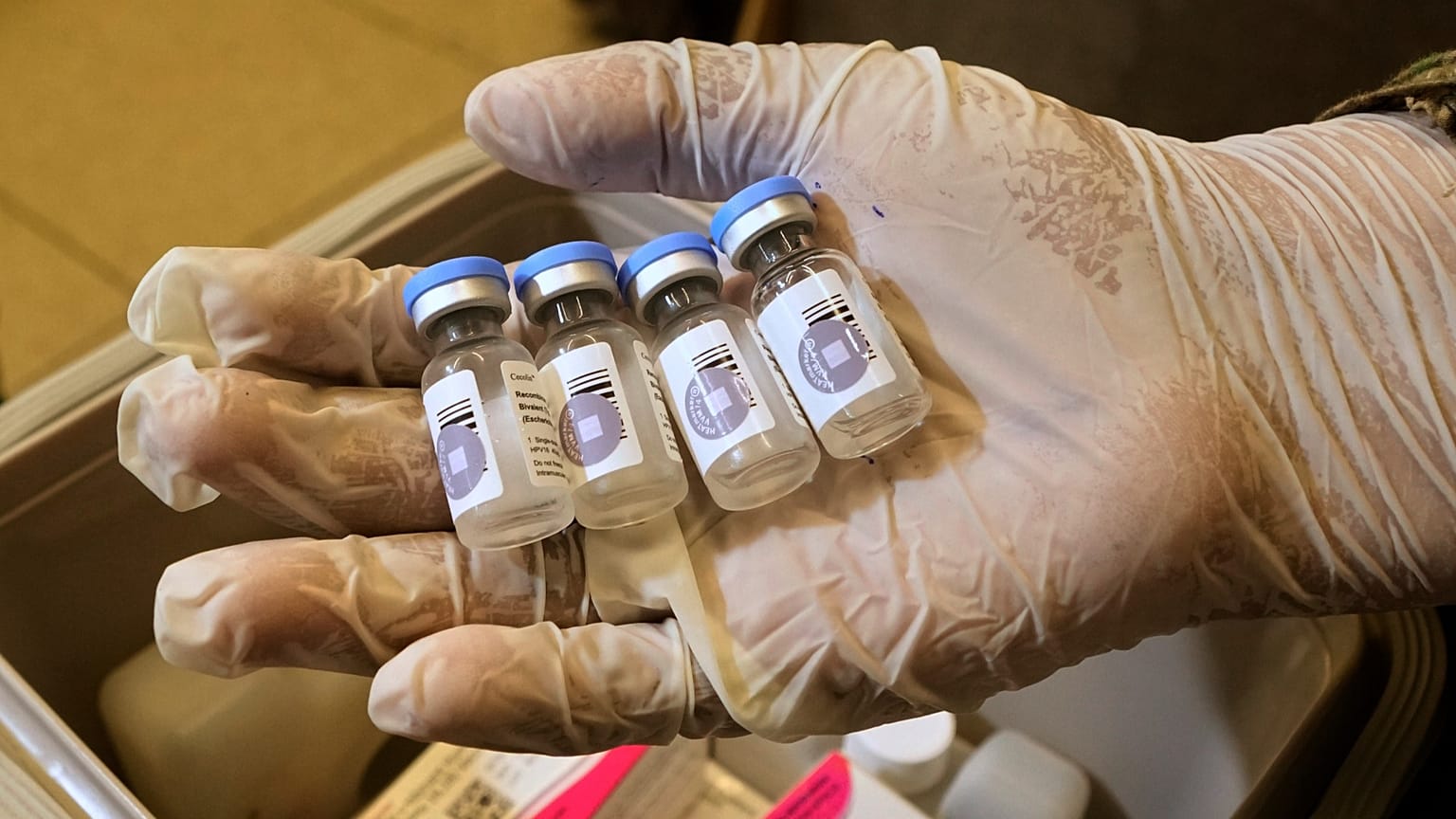
HPV vaccines such as Cervarix and Gardasil have been hailed as a major medical breakthrough in the fight against cervical cancer since their launch in the early 2000s – but they have also been controversial.
Merck & Co, which makes Gardasil, has faced lawsuits for years that allege the company wrongfully marketed the jab as safe when it actually caused heart rate changes and fertility problems. Earlier this year, a US judge ruled in Merck’s favour, saying those claims were “speculative inferences”.
Over the past decade, HPV vaccination rates have risen steadily in some European countries – such as Spain and Germany – but fallen in places like the United Kingdom and Italy, according to WHO data.
The Cochrane researchers cited social media misinformation as a key driver of falling or stagnant immunisation rates, and set out to identify whether those concerns had merit.
“We think it's really important that we have an independent, comprehensive view of the literature so we can provide evidence … in a way that can help people make informed choices to improve their health,” Dr Jo Morrison, one of the study’s authors and a gynaecological oncologist, told journalists during a briefing.
Her team found that HPV jabs only cause minor side effects, such as a sore arm right after vaccination. After checking reports of serious safety concerns against real-world follow-up data, they found no evidence that vaccination raises these risks.
Serious side effects were rare and were equally likely to occur in groups of people who had not been vaccinated.
“An important finding was that the commonly reported side effects of the vaccine, often discussed on social media, were found to hold no evidence of a real link to vaccination,” Henschke said.
Findings support vaccination
The researchers said the findings support global guidance for both girls and boys to get vaccinated against HPV, ideally before they turn 16. People are most protected when they are vaccinated before they are exposed to the virus or become sexually active, they said.
While the HPV vaccine was initially only recommended for girls and women, countries are increasingly also targeting boys.
“Vaccinating boys as well as girls boosts protection for everyone,” Morrison said. “Over time we’ll see the impact of vaccination on other cancers too, including ones that affect men”.
The Cochrane team pointed to some gaps in the evidence base on HPV vaccination. For example, most studies were done in wealthy countries, meaning more research is needed in lower-income countries where the cervical cancer burden is higher.
The researchers expect to learn more in the coming years about how the HPV jab affects other cancers linked to the virus, which tend to develop later in life.
“It will take decades to fully understand the impact of vaccination,” Morrison said.